Understanding this New Keratome
This section is for surgeons prior to using curved, multi-pionted keratomes. In essence, this type of keratome uses the same cutting principles like other keratomes, but with some unique features:
Tips
Because the tip of the blade does the work in making the
important parts of the (biplanar) incision, multiple connected tips
multiply the work in making multiple connected parts of the incision -
the first part of the incision parallel to the iris plane and the
internal flap. The net result from using this new keratome is
an incision where the entire width of the keratome blade passes
completely through the cornea for the entire length of the (2.0mm)
incision, making a complete tunnel of uniform width.
Dr. I.H. Fine showed that linear incisions made in the plane of the cornea were found to be arcuate by optical coherence tomography (OCT), creating a tongue-and-goove-like fit of the floor to the roof of the incision appearing to add greater stability, and concluded that an incision length of at least 2.0 mm provided advantageous architecture for adequate self-sealing (Profile of clear corneal cataract incisions demonstrated by ocular coherence tomography. J Cataract Refract Surg. 2007 Jan;33(1):94-7). About Linear-to-Arcuate Incisions.
As known in surgery and consistent with the scaled CAD
simulation of these incisions, a 2.0mm incision length made in the
plane of the cornea with a flat, single-pointed blade risks injury to
the central cornea, requiring a more shallow angle toward the end of
the incision that may contribute to an arcuate incision along the
sides. However, by geometry, a curved, dual-pointed keratome
will make the same width of the incision at half the depth, allowing
these incisions to be truly linear and to be made more safely.
These arcuate findings are supported by an engineering analysis (ESCRS 2003) - when the incision is made, the static equilibrium changes to a dynamic state where bonds are broken, the cornea exerts less force against the IOP, and the cornea moves outward as the incision is made, creating an arcuate-type incision. Since the tip of the blade performs the work in making these incisions (where the forces are isolated), multiple tips will create multiple tongue-and-goove-like fittings, similar to dovetails in furniture making, further enhancing the stability and sealing of the incision.
In addition to these linear-to-arcuate-type incisions, multiple thin internal flaps may also be made with a keratome with multiple tips to further enhance the sealing under low IOPs:
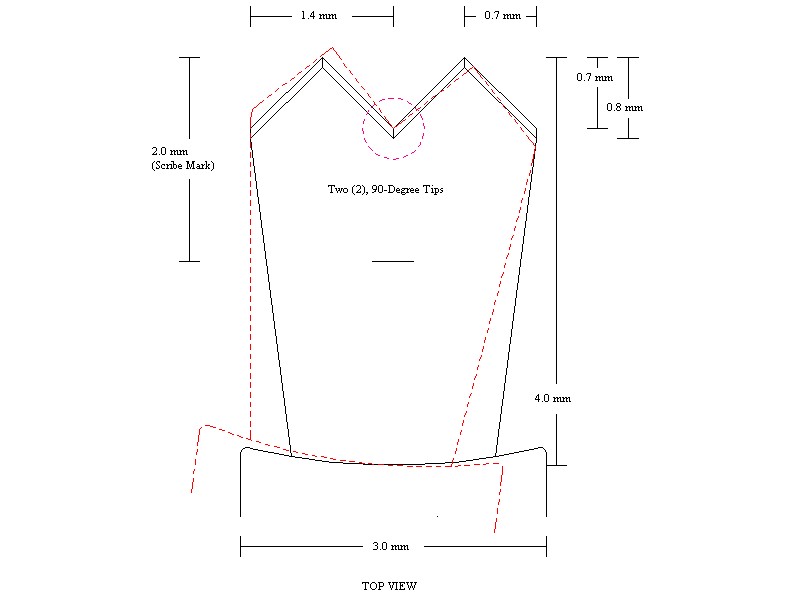
Valley. Because the valley of the blade is the connecting part for the tips that also cuts the cornea, a sharp V-shaped valley is as important as having sharp tips.
More Force. Keep in mind that more tips will require more force to make the incision, and that sufficient counter-pressure is a principle in surgery from sufficient inflation of the globe. Similarly, slightly less sharply pointed tips, such as these 90-degree tips, will also require slightly more force.
LIMITATION. Because this keratome was initially designed primarily for larger IOL implantation by making wider (and/or more effective) self-sealing corneal incisions where a complete tunnel of uniform width is made through the entire length of the incision (as compared to the typical flat, single-pointed keratomes), "oar locking" may be a concern, especially during phaco, where circulation of the cooling fluid may be restricted that may cause corneal burns.
Benefit for Surgeons. Because a principle in surgery is to make incisions of sufficient size to adequately perform the procedure, it is reasonable that this new keratome, designed to produce more effective, self-sealing corneal incisions, will allow more adequately-sized incisions for procedures without the higher risk for infections.
In the OR
- Inspect
the keratome
(especially for sharpness of the blade's tips, valley and edges).
- Insure good Inflation
of the
globe.
- Apply the necessary Counter-Pressure.
A recommended technique is to use two fingers on the contralateral side
of the incision [which disperses the force in making the incision over
the two fingers in contact with the cornea]. Using a forcep adjacent to
the incision tends to concentrate this greater force over this single
point, which may tear tissue.
- When the Valley of the blade
disappears under the cornea epithelium, the tips are at a depth of
0.7-0.8mm, providing an indication to change the angle the incision.
- A 2.0mm Scribe Mark is also
provided as a depth gauge to enter the anterior chamber.
- Should more Resistance be
encountered when making the incision, particularly when penetrating
(thicker) Descemet's Membrane, THEN a slight left-to-right rotation or
"WIGGLE" of the heel of the blade with constant pressure may provide
the necessary cutting action. (Note: The same force is now applied over
one half of the blade, which will provide better cutting action.)
- Good surgeons always maintain control, so one should keep in perspective the incision and anatomy and Not Rely on the mechanical Safety Stop.